Post-Transplant Ankylosing Spondylitis Case Report
The appearance of inflammatory and autoimmune diseases is quite low in patients after solid organ transplantation. Adequate immunosuppressive therapy usually mitigates the risk of relapse or new onset of autoimmune disease in this population. Dr. Zawiasa-Bryszewska Anna of the Medical University of Lodz, Poland, and team have recently reported a case of post-transplant ankylosing spondylitis (AK) in a 58-year-old woman. The case report has been published in the journal BMC Nephrology on January 31, 2021.
The clinical presentation of inflammatory diseases in patients after transplantation is commonly atypical and often leads to delayed diagnosis. Ankylosing spondylitis (AS), previously known as Bechterew's disease, is a chronic, progressive inflammatory disease with a diverse clinical presentation. The authors reported a case of late-onset seronegative spondyloarthropathy in a kidney transplant (KTx) patient despite ongoing immunosuppressive treatment.
Case Details
The authors described a 58-year-old female patient with end-stage renal disease caused by chronic glomerulonephritis, with a previous history of allogenic KTx 25 years earlier. She was on chronic immunosuppressive therapy based on cyclosporine A (CsA), mycophenolate mofetil (MMF), and prednisone, with no previous history of connective tissue disease. She was admitted to the hospital with a fever up to 39 °C and pain localized in the sacroiliac region radiating to the left lower limb for 2 weeks. Her vitals were stable. Initial blood works were normal with elevated CRP levels (287 mg/l) and urinalysis showed proteinuria 0.1 g/l. The doctors noted a stable graft function. Echo findings, urine and blood culture, and other viral tests were negative. The physicians administered empiric antibiotic therapy with clindamycin. They examined the Nuclear magnetic resonance (NMR) of the lumbar spine which was inconclusive, although the patient complained of constant pain aggravation.
On the tenth day of hospitalization, physicians observed oedema with tenderness of the left knee. They performed arthrocentesis and withdrew sixty millilitres of turbid fluid. They found the presence of Streptococcus sp. (saprophytic flora) in synovial fluid. So, they started prolonged targeted vancomycin therapy. Despite antibiotic treatment, further high inflammation parameters were still noted (CRP 149.4 mg/l), thus further diagnosis for atypical infection was performed. Further analysis of synovial fluid was also negative.
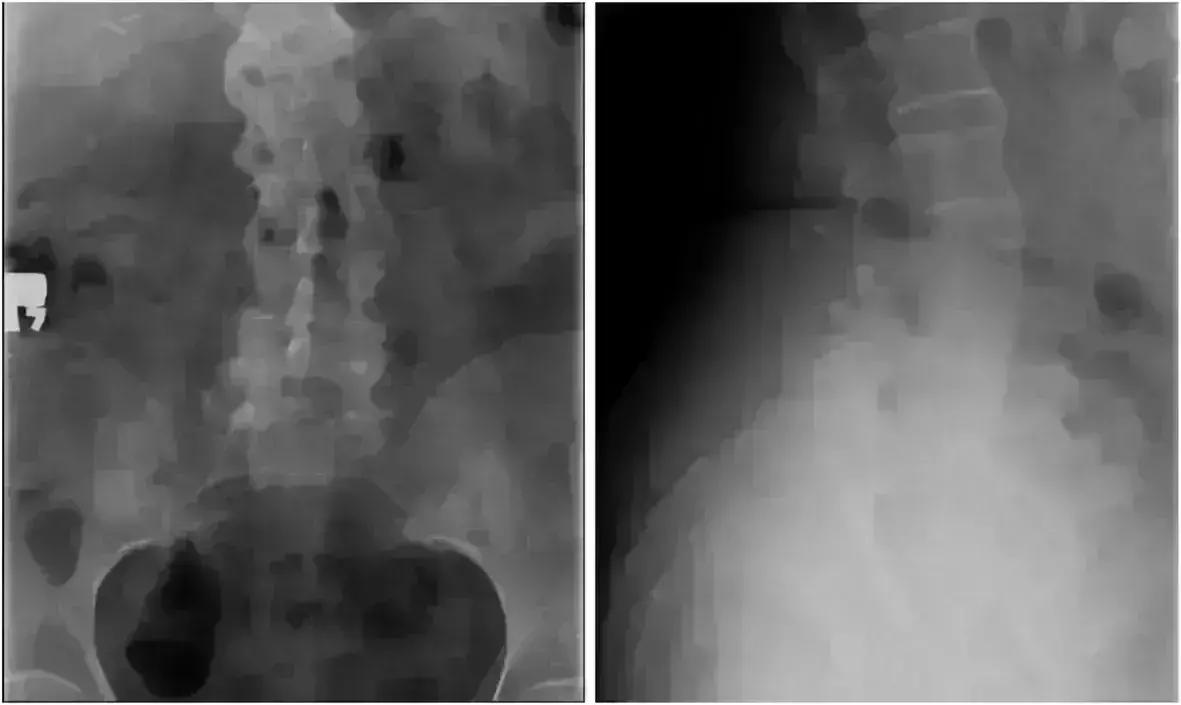
After the failure of treatment and the patient's continuing complaints, they referred the patient to the Department of Rheumatology. The patient was presented with left knee pain sustained for more than a month and lumbar spine pain, severity independent of physical exercise, exacerbating during the night and accompanied by morning stiffness. Joint mobility was within the normal range, soreness during loading, and maximum limbs bent with positive Patrick sign on the left side. After more detailed anamnesis, the patient confirmed the occurrence of typical inflammatory back pain of nearly 20 years. Detailed diagnostic procedures and x-rays of the lumbar spine and the targeted sacroiliac joints revealed lesions characteristic of AS: vertebral body squaring, diffuse syndesmophyitic ankyloses giving a "bamboo spine" appearance, and total ankyloses of sacroiliac joints. A diagnosis of ankylosing spondylitis was posed and the patient received oral sulphasalazine and NSAIDs. The treatment resulted in a significant decrease in CRP and improvement of the graft function. Radiosynovectomy in the left knee joint was performed and after 2 weeks, the patient was in good general condition and discharged to home.
The authors concluded, "The establishing of proper diagnosis and management of a patient after KTx is difficult. Despite long-term immunosuppressive treatment in solid organ transplant recipients, in the differential diagnosis of joint pain, the development of de novo arthritis should be considered, and when conclusive diagnosis is made, the patient may require administration of additional immunosuppressive drugs".


0 Comments
Post a comment
No comments yet. Be the first to comment!