Bariatric Surgery May Worsen Existing Serious Diabetic Retinopathy: Study
- byDoctor News Daily Team
- 07 July, 2025
- 0 Comments
- 0 Mins
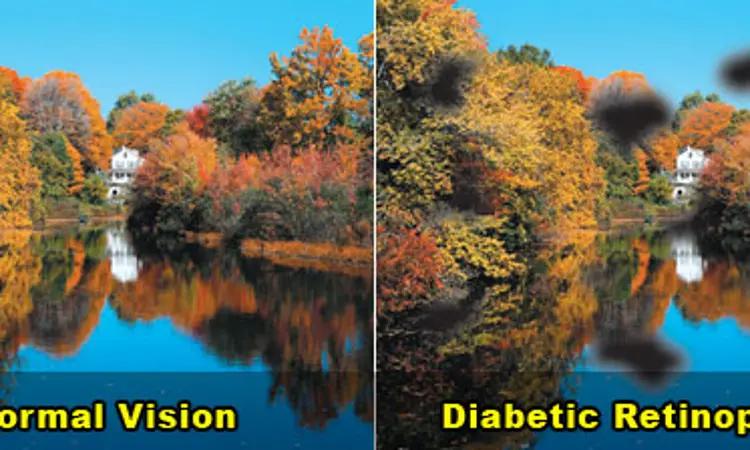
Morbid obesity is a major problem in developed societies; it is responsible for decreased expectancy and quality of life and leads to multiple comorbid conditions. Bariatric surgery is becoming increasingly popular with the rising prevalence of obesity.While bariatric surgery induces remission of type 2 diabetes mellitus and reduces other microvascular complications, its impact on diabetic retinopathy (DR) is unclear.
Researchers have found in a new study that while bariatric surgery was associated with fewer cases of all and sight-threatening DR, early worsening was more severe in patients with existing sight-threatening DR.
The study findings were published in the American Journal of Ophthalmology on January 08, 2021.
Recently, bariatric surgery has been recognised not only as an effective treatment for achieving substantial sustained weight loss but also in inducing significant and rapid glycaemic control resulting in remission of type 2 diabetes in approximately 80% of cases within 2 years. Therefore, NICE has recommended bariatric surgery as a treatment option for obese patients with type 2 diabetes who are refractory to other weight-loss management options. However, little is known about the effect of bariatric surgery on diabetic microvascular complications such as diabetic retinopathy (DR). Some trials suggest early worsening of DR post-surgery due to rapid hyperglycemia improvements. Therefore, researchers of Ontario, Canada, conducted a meta-analysis to estimate the impact of bariatric surgery on DR for obese patients in comparison to medical treatment.
It was a systemic review and meta-analysis. Researchers used MEDLINE, EMBASE, and CENTRAL databases for primary studies comparing DR in patients undergoing bariatric surgery to medical management and included a total of 14 studies comprised of 110,300 surgical and 252,289 control patients. They used a random-effects model for the meta-analysis results. The major outcome assessed was the prevalence of all DR and sight-threatening DR after surgery. They also assessed the worsening of DR within and beyond 12 months.
Upon analysis, researchers noted that surgical patients had statistically significantly lower post-operative prevalence of all DR (RR 0.17) and sight-threatening DR (RR 0.47). They found early worsening of DR and progression to sight-threatening DR had occurred more often in those with more severe DR initially. They also found after 2 months, the bariatric surgery resulted in significantly fewer patients with worsened DR (RR 0.29). They reported that the overall risk of bias was low and the estimates of relative effects had low to moderate certainty of evidence.
The authors concluded, "While bariatric surgery was associated with fewer cases of all and sight-threatening DR, early worsening was more severe in patients with existing sight-threatening DR. These findings argue for frequent monitoring during the first post-operative year".
For further information:
https://www.ajo.com/article/S0002-9394(21)00007-6/fulltext#%20
Disclaimer: This website is designed for healthcare professionals and serves solely for informational purposes.
The content provided should not be interpreted as medical advice, diagnosis, treatment recommendations, prescriptions, or endorsements of specific medical practices. It is not a replacement for professional medical consultation or the expertise of a licensed healthcare provider.
Given the ever-evolving nature of medical science, we strive to keep our information accurate and up to date. However, we do not guarantee the completeness or accuracy of the content.
If you come across any inconsistencies, please reach out to us at
admin@doctornewsdaily.com.
We do not support or endorse medical opinions, treatments, or recommendations that contradict the advice of qualified healthcare professionals.
By using this website, you agree to our
Terms of Use,
Privacy Policy, and
Advertisement Policy.
For further details, please review our
Full Disclaimer.
Recent News
Gum disease could silently cause serious brain dam...
- 03 November, 2025
Can Early-Day Fasting Significantly Boost Metaboli...
- 03 November, 2025
Delhi HC bars doctor from running medical centre d...
- 03 November, 2025
Phase III data for Gazyva/Gazyvaro show significan...
- 03 November, 2025
Daily Newsletter
Get all the top stories from Blogs to keep track.


0 Comments
Post a comment
No comments yet. Be the first to comment!